
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
- Trends in the Prevalence of Obesity and Its Phenotypes Based on the Korea National Health and Nutrition Examination Survey from 2007 to 2017 in Korea
- Sang Ouk Chin, You-Cheol Hwang, Hong-Yup Ahn, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
- Diabetes Metab J. 2022;46(5):808-812. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0226
- 3,923 View
- 216 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - This study used data from the Korea National Health and Nutrition Examination Survey IV–VII from 2007 to identify the prevalence of obesity and its phenotypes (metabolically unhealthy obesity [MUO] and metabolically healthy obesity [MHO]) and their secular changes. The prevalence of obesity in Korea increased with significant secular changes observed (β=0.326, P trend <0.01) between 2007 and 2017, and especially in men (β=0.682, P trend <0.001) but not in women. The changes in the prevalence of obesity during the study period were different between men and women (P=0.001). The prevalence of MUO significantly increased only in men (β=0.565, P trend <0.01), while that of MHO increased only in women (β=0.179, P<0.05), especially in the younger age group (β=0.308, P<0.01).
-
Citations
Citations to this article as recorded by- Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - Differences of Regional Fat Distribution Measured by Magnetic Resonance Imaging According to Obese Phenotype in Koreans
Ha-Neul Choi, Hyunjung Lim, Young-Seol Kim, Sang-Youl Rhee, Jung-Eun Yim
Metabolic Syndrome and Related Disorders.2022; 20(10): 551. CrossRef
- Hormonal Gut–Brain Signaling for the Treatment of Obesity
- Drug/Regimen
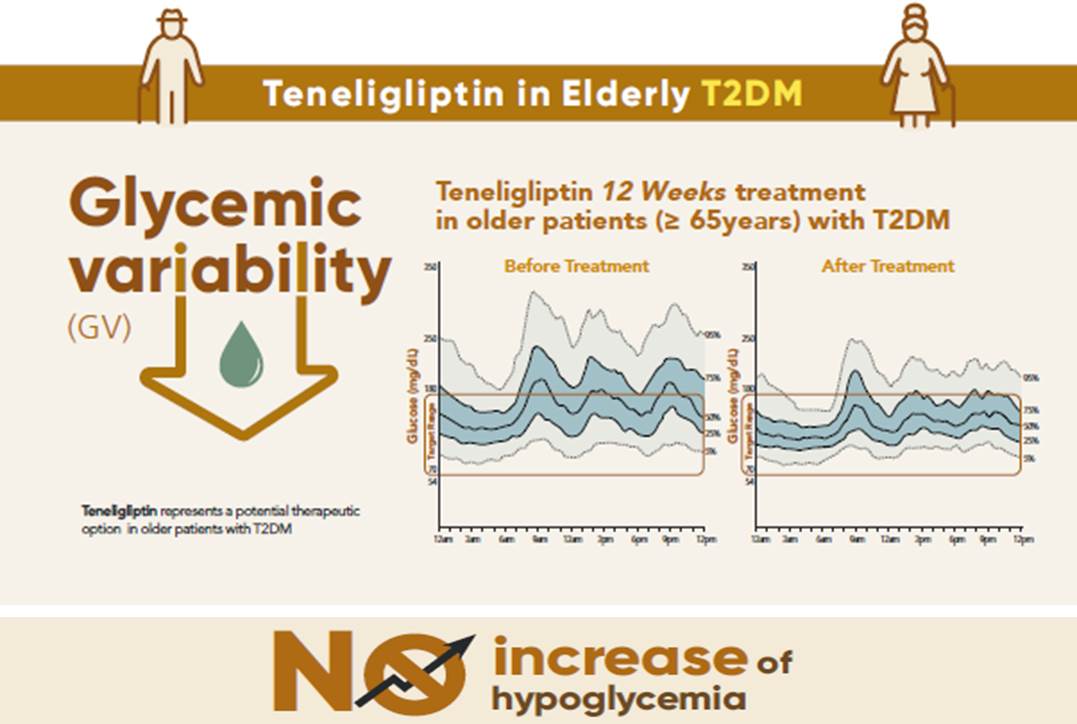
- Effects of Teneligliptin on HbA1c levels, Continuous Glucose Monitoring-Derived Time in Range and Glycemic Variability in Elderly Patients with T2DM (TEDDY Study)
- Ji Cheol Bae, Soo Heon Kwak, Hyun Jin Kim, Sang-Yong Kim, You-Cheol Hwang, Sunghwan Suh, Bok Jin Hyun, Ji Eun Cha, Jong Chul Won, Jae Hyeon Kim
- Diabetes Metab J. 2022;46(1):81-92. Published online June 16, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0016
- 7,586 View
- 431 Download
- 5 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 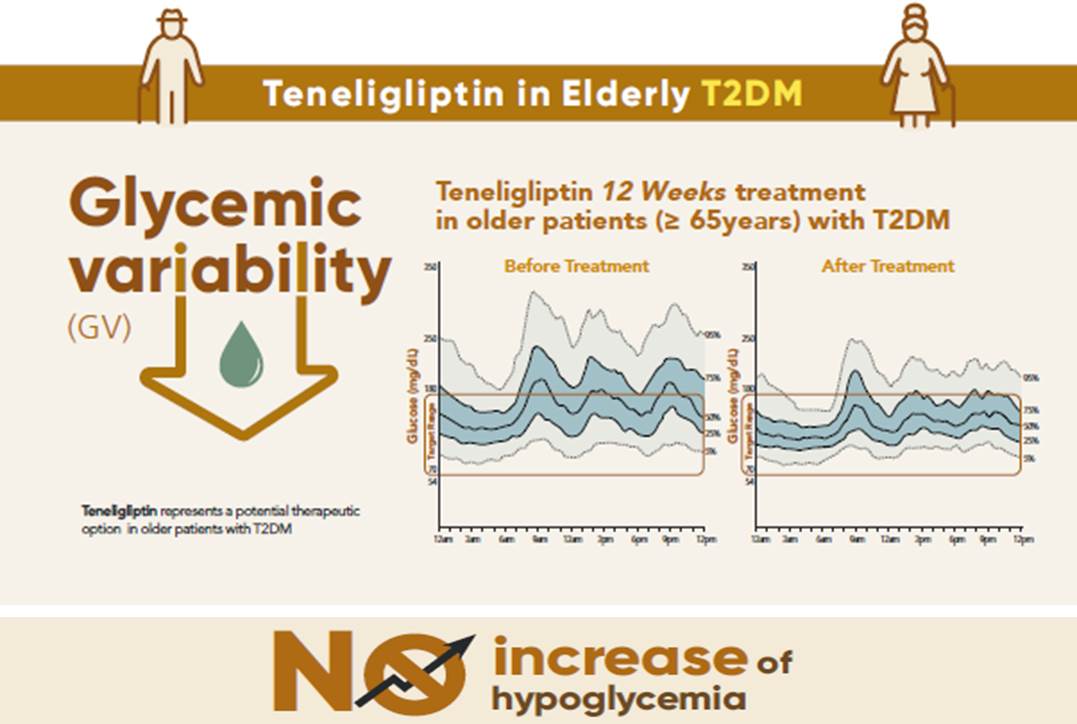
- Background
To evaluate the effects of teneligliptin on glycosylated hemoglobin (HbA1c) levels, continuous glucose monitoring (CGM)-derived time in range, and glycemic variability in elderly type 2 diabetes mellitus patients.
Methods
This randomized, double-blinded, placebo-controlled study was conducted in eight centers in Korea (clinical trial registration number: NCT03508323). Sixty-five participants aged ≥65 years, who were treatment-naïve or had been treated with stable doses of metformin, were randomized at a 1:1 ratio to receive 20 mg of teneligliptin (n=35) or placebo (n=30) for 12 weeks. The main endpoints were the changes in HbA1c levels from baseline to week 12, CGM metrics-derived time in range, and glycemic variability.
Results
After 12 weeks, a significant reduction (by 0.84%) in HbA1c levels was observed in the teneligliptin group compared to that in the placebo group (by 0.08%), with a between-group least squares mean difference of –0.76% (95% confidence interval [CI], –1.08 to –0.44). The coefficient of variation, standard deviation, and mean amplitude of glycemic excursion significantly decreased in participants treated with teneligliptin as compared to those in the placebo group. Teneligliptin treatment significantly decreased the time spent above 180 or 250 mg/dL, respectively, without increasing the time spent below 70 mg/dL. The mean percentage of time for which glucose levels remained in the 70 to 180 mg/dL time in range (TIR70–180) at week 12 was 82.0%±16.0% in the teneligliptin group, and placebo-adjusted change in TIR70–180 from baseline was 13.3% (95% CI, 6.0 to 20.6).
Conclusion
Teneligliptin effectively reduced HbA1c levels, time spent above the target range, and glycemic variability, without increasing hypoglycemia in our study population. -
Citations
Citations to this article as recorded by- Comparison of teneligliptin and other gliptin-based regimens in addressing insulin resistance and glycemic control in type 2 diabetic patients: a cross-sectional study
Harmanjit Singh, Ravi Rohilla, Shivani Jaswal, Mandeep Singla
Expert Review of Endocrinology & Metabolism.2024; 19(1): 81. CrossRef - Potential approaches using teneligliptin for the treatment of type 2 diabetes mellitus: current status and future prospects
Harmanjit Singh, Jasbir Singh, Ravneet Kaur Bhangu, Mandeep Singla, Jagjit Singh, Farideh Javid
Expert Review of Clinical Pharmacology.2023; 16(1): 49. CrossRef - Mechanism of molecular interaction of sitagliptin with human DPP4 enzyme - New Insights
Michelangelo Bauwelz Gonzatti, José Edvar Monteiro Júnior, Antônio José Rocha, Jonathas Sales de Oliveira, Antônio José de Jesus Evangelista, Fátima Morgana Pio Fonseca, Vânia Marilande Ceccatto, Ariclécio Cunha de Oliveira, José Ednésio da Cruz Freire
Advances in Medical Sciences.2023; 68(2): 402. CrossRef - A prospective multicentre open label study to assess effect of Teneligliptin on glycemic control through parameters of time in range (TIR) Metric using continuous glucose monitoring (TOP-TIR study)
Banshi Saboo, Suhas Erande, A.G. Unnikrishnan
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(2): 102394. CrossRef - Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
Min Jeong Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2022; 46(1): 49. CrossRef
- Comparison of teneligliptin and other gliptin-based regimens in addressing insulin resistance and glycemic control in type 2 diabetic patients: a cross-sectional study
- Metabolic Risk/Epidemiology
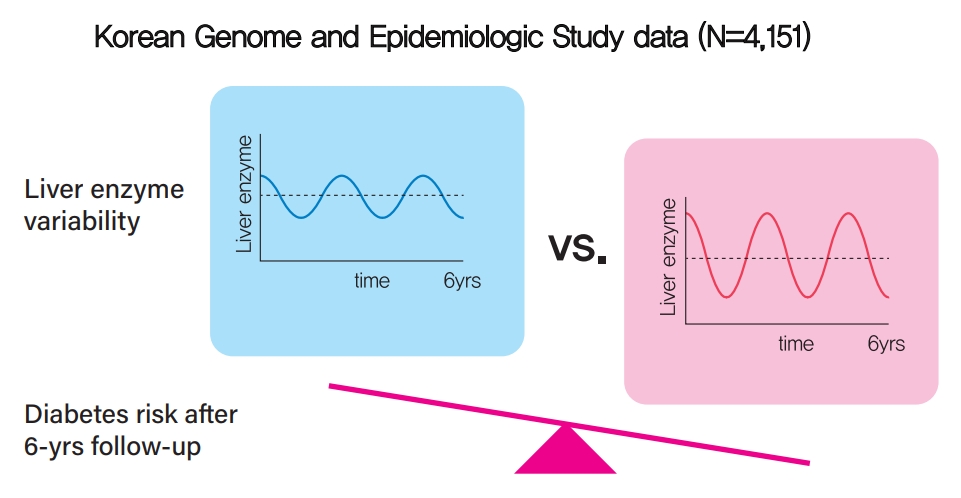
- Increased Visit-to-Visit Liver Enzyme Variability Is Associated with Incident Diabetes: A Community-Based 12-Year Prospective Cohort Study
- Kyuhoon Bang, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung, You-Cheol Hwang
- Diabetes Metab J. 2021;45(6):890-898. Published online March 17, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0208
- 4,825 View
- 155 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 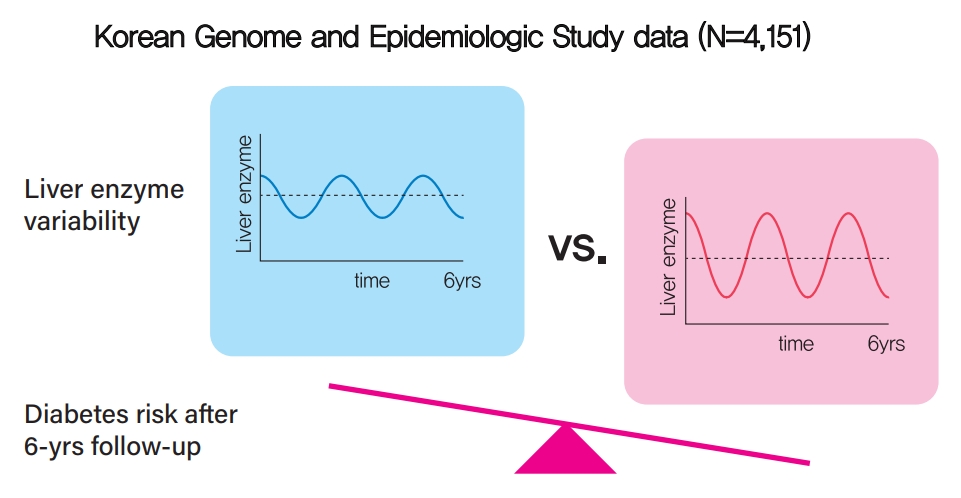
- Background
Fatty liver and/or increased liver enzyme values have been reported to be associated with incident diabetes. We sought to determine whether increased visit-to-visit liver enzyme variability is associated with incident diabetes.
Methods
Study participants were recruited from the Korean Genome and Epidemiologic Study (KoGES). A total of 4,151 people aged 40 to 69 years was recruited and tested every 2 years for up to 12 years. Visit-to-visit aspartate aminotransferase (AST) and alanine aminotransferase (ALT) variability was evaluated in first the 6-year period through the use of various variability measurements: standard deviation (SD), average successive variability, coefficient of variation (CV), and variation independent of mean (VIM). Oral glucose tolerance test was performed at every visit.
Results
During the 6-year follow‐up appointments, 13.0% (538/4,151) of people developed incident diabetes. Visit-to-visit AST variability was associated with an increased risk of diabetes independent of conventional risk factors for diabetes (hazard ratio per 1-SD increment [95% confidence interval]: 1.06 [1.00 to 1.11], 1.12 [1.04 to 1.21], and 1.13 [1.04 to 1.22] for SD, CV, and VIM, respectively; all P<0.05); however, no such associations were observed in the visit-to-visit ALT variability. According to alcohol consumption status, both AST and ALT variability were independent predictors for incident diabetes in subjects with heavy alcohol consumption; however, neither AST nor ALT variability was associated with diabetes risk in subjects who did not drink alcohol heavily.
Conclusion
Visit-to-visit liver enzyme variability is an independent predictor of incident diabetes. Such association was more evident in those who consumed significant amounts of alcohol.
- Metabolic Risk/Epidemiology
- Intra-Abdominal Fat and High Density Lipoprotein Cholesterol Are Associated in a Non-Linear Pattern in Japanese-Americans
- Sun Ok Song, You-Cheol Hwang, Steven E. Kahn, Donna L. Leonetti, Wilfred Y. Fujimoto, Edward J. Boyko
- Diabetes Metab J. 2020;44(2):277-285. Published online March 10, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0008
- 4,678 View
- 63 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We describe the association between high density lipoprotein cholesterol (HDL-C) concentration and computed tomography (CT)-measured fat depots.
Methods We examined the cross-sectional associations between HDL-C concentration and intra-abdominal (IAF), abdominal subcutaneous (SCF), and thigh fat (TF) areas in 641 Japanese-American men and women. IAF, SCF, and TF were measured by CT at the level of the umbilicus and mid-thigh. The associations between fat area measurements and HDL-C were examined using multivariate linear regression analysis adjusting for age, sex, diabetes family history, homeostasis model assessment of insulin resistance (HOMA-IR), and body mass index (BMI). Non-linearity was assessed using fractional polynomials.
Results Mean±standard deviation of HDL-C concentration and IAF in men and women were 1.30±0.34 mg/dL, 105±55.3 cm2, and 1.67±0.43 mg/dL, 74.4±46.6 cm2 and differed significantly by gender for both comparisons (
P <0.001). In univariate analysis, HDL-C concentration was significantly associated with CT-measured fat depots. In multivariate analysis, IAF was significantly and non-linearly associated with HDL-C concentration adjusted for age, sex, BMI, HOMA-IR, SCF, and TF (IAF: β=−0.1012, P<0.001; IAF2: β=0.0008,P <0.001). SCF was also negatively and linearly associated with HDL-C (β=−0.4919,P =0.001).Conclusion HDL-C does not linearly decline with increasing IAF in Japanese-Americans. A more complex pattern better fits this association.
-
Citations
Citations to this article as recorded by- Associations of Serum Uric Acid to High-Density Lipoprotein Cholesterol Ratio with Trunk Fat Mass and Visceral Fat Accumulation
Yansu Wang, Yiting Xu, Tingting Hu, Yunfeng Xiao, Yufei Wang, Xiaojing Ma, Haoyong Yu, Yuqian Bao
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 121. CrossRef - Obesity-related parameters in carriers of some BDNF genetic variants may depend on daily dietary macronutrients intake
Urszula Miksza, Edyta Adamska-Patruno, Witold Bauer, Joanna Fiedorczuk, Przemyslaw Czajkowski, Monika Moroz, Krzysztof Drygalski, Andrzej Ustymowicz, Elwira Tomkiewicz, Maria Gorska, Adam Kretowski
Scientific Reports.2023;[Epub] CrossRef - Computed tomography-based investigation of the correlation of abdominal fat areas with metabolic syndrome
Kai-Yuan Cheng, Tsung-Hsien Yen, Jay Wu, Pei-Hsuan Li, Tian-Yu Shih
Journal of Radiological Science.2023; 48(1): 15. CrossRef - Lower High-Density Lipoprotein Cholesterol Concentration Is Independently Associated with Greater Future Accumulation of Intra-Abdominal Fat
Sun Ok Song, You-Cheol Hwang, Han Uk Ryu, Steven E. Kahn, Donna L. Leonetti, Wilfred Y. Fujimoto, Edward J. Boyko
Endocrinology and Metabolism.2021; 36(4): 835. CrossRef
- Associations of Serum Uric Acid to High-Density Lipoprotein Cholesterol Ratio with Trunk Fat Mass and Visceral Fat Accumulation
- Response: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (
Diabetes Metab J 2019;43:582–9) - You-Cheol Hwang
- Diabetes Metab J. 2019;43(6):915-916. Published online December 26, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0213
- 2,577 View
- 44 Download
- 1 Crossref
-
 PDF
PDF PubReader
PubReader -
Citations
Citations to this article as recorded by- Improved Pharmacodynamic Potential of Rosuvastatin by Self-Nanoemulsifying Drug Delivery System: An in vitro and in vivo Evaluation
Ravinder Verma, Ajeet Kaushik, Rafa Almeer, Md Habibur Rahman, Mohamed M Abdel-Daim, Deepak Kaushik
International Journal of Nanomedicine.2021; Volume 16: 905. CrossRef
- Improved Pharmacodynamic Potential of Rosuvastatin by Self-Nanoemulsifying Drug Delivery System: An in vitro and in vivo Evaluation
- Clinical Diabetes & Therapeutics
- A Lower Baseline Urinary Glucose Excretion Predicts a Better Response to the Sodium Glucose Cotransporter 2 Inhibitor
- You-Cheol Hwang, Jae Hyeon Kim, Byung-Wan Lee, Woo Je Lee
- Diabetes Metab J. 2019;43(6):898-905. Published online June 14, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0257
- 3,935 View
- 80 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader We aimed to identify the clinical variables associated with a better glucose-lowering response to the sodium glucose cotransporter 2 inhibitor ipragliflozin in people with type 2 diabetes mellitus (T2DM). We especially focused on urinary glucose excretion (UGE). This was a single-arm multicenter prospective study. A total of 92 people with T2DM aged 20 to 70 years with glycosylated hemoglobin (HbA1c) levels ≥7.0% and ≤9.5% were enrolled. Ipragliflozin (50 mg) was added to the background therapy for these people for 12 weeks. After 3 months treatment with ipragliflozin, the mean HbA1c levels were decreased from 7.6% to 6.9% and 62.0% of the people reached the HbA1c target of less than 7.0% (
P <0.001). In addition, body weight, blood pressure, and lipid parameters were improved after ipragliflozin treatment (allP <0.001). The baseline HbA1c (r =0.66,P <0.001) and morning spot urine glucose to creatinine ratio (r =−0.30,P =0.001) were independently associated with the HbA1c reduction. Ipragliflozin treatment for 12 weeks improves glycemic control and other metabolic parameters. A higher HbA1c and lower UGE at baseline predicts a better glucose-lowering efficacy of ipragliflozin.-
Citations
Citations to this article as recorded by- Preventing and Treating Metabolic Dysfunction-Associated Steatotic Liver Disease in People with Type 2 Diabetes: Promising Therapeutic Agents and Strategies
Allison Zhang, Rita El Hachem, Jennifer Goldman
ADCES in Practice.2024; 12(1): 38. CrossRef - Association of common variant rs9934336 of SLC5A2 (SGLT2) gene with SARS-CoV-2 infection and mortality
Anamika Das, Gunanidhi Dhangadamajhi
Egyptian Journal of Medical Human Genetics.2024;[Epub] CrossRef - Mathematical Models of the Effect of Glucagon on Glycemia in Individuals With Type 2 Diabetes Treated With Dapagliflozin
Tomoko Yamada, Hikaru Sugimoto, Ken-ichi Hironaka, Yasuko Morita, Hiroshi Miura, Natsu Otowa-Suematsu, Yuko Okada, Yushi Hirota, Kazuhiko Sakaguchi, Shinya Kuroda, Wataru Ogawa
Journal of the Endocrine Society.2024;[Epub] CrossRef - β-hydroxybutyrate as a biomarker of β-cell function in new-onset type 2 diabetes and its association with treatment response at 6 months
Minyoung Lee, Yongin Cho, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-Wan Lee
Diabetes & Metabolism.2023; 49(4): 101427. CrossRef - A Comparative Study on the Efficacy and Safety of Dose Escalation of Luseogliflozin in Type 2 Diabetes Mellitus Patients With Poor Glycemic Control
Tadashi Arao, Yosuke Okada, Akira Kurozumi, Yoshiya Tanaka
Cureus.2023;[Epub] CrossRef - Role of SLC5A2 polymorphisms and effects of genetic polymorphism on sodium glucose cotransporter 2 inhibitors response
Bo Xu, Shaoqian Li, Bo Kang, Shangzhi Fan, Canyu Chen, Weiyi Li, Jixiang Chen, Zunbo He, Fan Tang, Jiecan Zhou
Molecular Biology Reports.2023; 50(11): 9637. CrossRef - Current Use and Complementary Value of Combining in Vivo Imaging Modalities to Understand the Renoprotective Effects of Sodium-Glucose Cotransporter-2 Inhibitors at a Tissue Level
Sjoukje van der Hoek, Jasper Stevens
Frontiers in Pharmacology.2022;[Epub] CrossRef - Clinical and genetic determinants of urinary glucose excretion in patients with diabetes mellitus
Keisuke Monobe, Shinsuke Noso, Naru Babaya, Yoshihisa Hiromine, Yasunori Taketomo, Fumimaru Niwano, Sawa Yoshida, Sara Yasutake, Tatsuro Minohara, Yumiko Kawabata, Hiroshi Ikegami
Journal of Diabetes Investigation.2021; 12(5): 728. CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef
- Preventing and Treating Metabolic Dysfunction-Associated Steatotic Liver Disease in People with Type 2 Diabetes: Promising Therapeutic Agents and Strategies
- Clinical Diabetes & Therapeutics
- Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus
- You-Cheol Hwang, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
- Diabetes Metab J. 2019;43(5):582-589. Published online January 16, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0124
- 6,612 View
- 185 Download
- 14 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The apolipoprotein B/A1 (apoB/A1) ratio is a stronger predictor of future cardiovascular disease than is the level of conventional lipids. Statin and ezetimibe combination therapy have shown additional cardioprotective effects over statin monotherapy.
Methods This was a single-center, randomized, open-label, active-controlled study in Korea. A total of 36 patients with type 2 diabetes mellitus were randomized to either rosuvastatin monotherapy (20 mg/day,
n =20) or rosuvastatin/ezetimibe (5 mg/10 mg/day,n =16) combination therapy for 6 weeks.Results After the 6-week treatment, low density lipoprotein cholesterol (LDL-C) and apoB reduction were comparable between the two groups (−94.3±15.4 and −62.0±20.9 mg/dL in the rosuvastatin group, −89.9±22.7 and −66.8±21.6 mg/dL in the rosuvastatin/ezetimibe group,
P =0.54 andP =0.86, respectively). In addition, change in apoB/A1 ratio (−0.44±0.16 in the rosuvastatin group and −0.47±0.25 in the rosuvastatin/ezetimibe group,P =0.58) did not differ between the two groups. On the other hand, triglyceride and free fatty acid (FFA) reductions were greater in the rosuvastatin/ezetimibe group than in the rosuvastatin group (−10.5 mg/dL [interquartile range (IQR), −37.5 to 29.5] and 0.0 µEq/L [IQR, −136.8 to 146.0] in the rosuvastatin group, −49.5 mg/dL [IQR, −108.5 to −27.5] and −170.5 µEq/L [IQR, −353.0 to 0.8] in the rosuvastatin/ezetimibe group,P =0.010 andP =0.049, respectively). Both treatments were generally well tolerated, and there were no differences in muscle or liver enzyme elevation.Conclusion A 6-week combination therapy of low-dose rosuvastatin and ezetimibe showed LDL-C, apoB, and apoB/A1 ratio reduction comparable to that of high-dose rosuvastatin monotherapy in patients with type 2 diabetes mellitus. Triglyceride and FFA reductions were greater with the combination therapy than with rosuvastatin monotherapy.
-
Citations
Citations to this article as recorded by- Moderate-Intensity Rosuvastatin/Ezetimibe Combination versus Quadruple-Dose Rosuvastatin Monotherapy: A Meta-Analysis and Systemic Review
Yura Kang, Jung Mi Park, Sang-Hak Lee
Yonsei Medical Journal.2024; 65(1): 19. CrossRef - Combination Therapy of Ezetimibe and Rosuvastatin for Dyslipidemia: Current Insights
Maya R Chilbert, Dylan VanDuyn, Sara Salah, Collin M Clark, Qing Ma
Drug Design, Development and Therapy.2022; Volume 16: 2177. CrossRef - Ezetimibe and diabetes mellitus:a new strategy for lowering cholesterol
V.A. Serhiyenko, A.A. Serhiyenko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(5): 302. CrossRef - The Effect of Rosuvastatin on Plasma/Serum Levels of High-Sensitivity C-Reactive Protein, Interleukin-6, and D-Dimer in People Living with Human Immunodeficiency Virus: A Systematic Review and Meta-Analysis
Akililu Alemu Ashuro, Yin-Guang Fan, Yuan-Sheng Fu, Dong-Sheng Di, Napoleon Bellua Sam, Hai-Feng Pan, Dong-Qing Ye
AIDS Research and Human Retroviruses.2021; 37(11): 821. CrossRef - Comparison of the Efficacy and Safety of Rosuvastatin/Ezetimibe Combination Therapy and Rosuvastatin Monotherapy on Lipoprotein in Patients With Type 2 Diabetes: Multicenter Randomized Controlled Study
Jiwoo Lee, You-Cheol Hwang, Woo Je Lee, Jong Chul Won, Kee-Ho Song, Cheol-Young Park, Kyu Jeung Ahn, Joong-Yeol Park
Diabetes Therapy.2020; 11(4): 859. CrossRef - Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis
Jaehyun Bae, Namki Hong, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Yong-ho Lee
Journal of Clinical Medicine.2020; 9(3): 798. CrossRef - Combined use of rosuvastatin and ezetimibe improves hepatic steatosis in patients with dyslipidemia
Won Dong Lee, Beom Kyung Kim, Jun Yong Park, Do Young Kim, Sang Hoon Ahn, Kwang-Hyub Han, Seung Up Kim
European Journal of Gastroenterology & Hepatology.2020; 32(12): 1538. CrossRef - Influence of rosuvastatin dose on total fatty acids and free fatty acids in plasma
Cristian I. Ciucanu, Sonia Olariu, Daliborca C. Vlad, Victor Dumitraşcu
Medicine.2020; 99(48): e23356. CrossRef - The effect of switching from statin-monotherapy to statin/ezetimibe combination therapy on lipid profiles in patients with type 2 diabetes and dyslipidemia: a multicenter open-label study (EUCLID)
Mitsuhide Takeshita, Atsushi Tanaka, Atsushi Kawaguchi, Keiko Sato, Shigeru Toyoda, Teruo Inoue, Koichi Node
Vascular Failure.2020; 4(1): 22. CrossRef - Response: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J 2019;43:582–9)
You-Cheol Hwang
Diabetes & Metabolism Journal.2019; 43(6): 915. CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - Changes in Plasma Free Fatty Acids Associated with Type-2 Diabetes
Amélie I. S. Sobczak, Claudia A. Blindauer, Alan J. Stewart
Nutrients.2019; 11(9): 2022. CrossRef
- Moderate-Intensity Rosuvastatin/Ezetimibe Combination versus Quadruple-Dose Rosuvastatin Monotherapy: A Meta-Analysis and Systemic Review
- Obesity and Metabolic Syndrome
- Higher High Density Lipoprotein 2 (HDL2) to Total HDL Cholesterol Ratio Is Associated with a Lower Risk for Incident Hypertension
- You-Cheol Hwang, Wilfred Y. Fujimoto, Steven E. Kahn, Donna L. Leonetti, Edward J. Boyko
- Diabetes Metab J. 2019;43(1):114-122. Published online September 28, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0053
- 4,248 View
- 46 Download
- 6 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recent studies have suggested that high density lipoprotein (HDL) cholesterol is inversely associated with the development of hypertension. We aimed to determine the association between different HDL cholesterol subclasses and risk of future hypertension.
Methods A total of 270 Japanese Americans (130 men, 140 women) without hypertension between the ages of 34 to 75 years were enrolled. Blood pressure was measured with a mercury sphygmomanometer, and average blood pressure was calculated. Incident hypertension was determined 5 to 6 and 10 to 11 years after enrollment. HDL2, HDL3, and total HDL cholesterol were measured at baseline.
Results During 10 years of follow-up, the cumulative incidence of hypertension was 28.1% (76/270). In univariate analysis, age, diabetes, waist circumference, systolic and diastolic blood pressure, fasting glucose, insulin resistance index, total and low density lipoprotein cholesterol, and visceral adipose tissue were significant predictors for incident hypertension. Among the HDL cholesterol subclass, HDL2 cholesterol was inversely associated with hypertension incidence, but both total and HDL3 cholesterol were not. In addition, HDL2/HDL cholesterol was inversely associated with future hypertension risk. In multivariate analysis, age (odds ratio [OR], 1.71; 95% confidence interval [CI], 1.26 to 2.31;
P =0.001), systolic blood pressure (OR, 1.83; 95% CI, 1.31 to 2.56;P <0.001), and HDL2/HDL cholesterol (OR, 0.71; 95% CI, 0.52 to 0.98;P =0.035), were associated with future development of hypertension.Conclusion A higher proportion of HDL2 cholesterol among total HDL cholesterol predicted a lower risk for incident hypertension. However, concentrations of total HDL, HDL2, and HDL3 cholesterol were not independent predictors of incident hypertension.
-
Citations
Citations to this article as recorded by- The Association of HDL2b with Metabolic Syndrome Among Normal HDL-C Populations in Southern China
Tong Chen, Shiquan Wu, Ling Feng, SiYu Long, Yu Liu, WenQian Lu, Wenya Chen, Guoai Hong, Li Zhou, Fang Wang, Yuechan Luo, Hequn Zou
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 363. CrossRef - Long-term PM1 exposure and hypertension hospitalization: A causal inference study on a large community-based cohort in South China
Yuqin Zhang, Shirui Chen, Jing Wei, Jie Jiang, Xiao Lin, Ying Wang, Chun Hao, Wenjing Wu, Zhupei Yuan, Jie Sun, Han Wang, Zhicheng Du, Wangjian Zhang, Yuantao Hao
Science Bulletin.2024;[Epub] CrossRef - High-Density Lipoprotein Signaling via Sphingosine-1-Phosphate Receptors Safeguards Spontaneously Hypertensive Rats against Myocardial Ischemia/Reperfusion Injury
Aishah Al-Jarallah, Fawzi A. Babiker
Pharmaceutics.2024; 16(4): 497. CrossRef - Effects of cardiometabolic risk factors on blood pressure in outpatients at Sominé DOLO hospital, Mopti, Mali
Modibo Coulibaly, Adama Kondé, Djibril Traoré, Ousmane Bah, Valentin Sagara, Bakary Maiga
International Journal of Clinical Biochemistry and Research.2023; 10(1): 87. CrossRef - The association of lipid metabolism with bone metabolism and the role of human traits: a Mendelian randomization study
Jian Kang, Shuangli Zhao, Xize Wu, Can Wang, Zongkun Jiang, Shixuan Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - The role of different lipid measures for incident hypertension during more than 12-year follow-up: Tehran Lipid and Glucose Study
Amirreza Hadaegh, Samaneh Akbarpour, Maryam Tohidi, Niloofar Barzegar, Somayeh Hosseinpour-Niazi, Fereidoun Azizi, Farzad Hadaegh
British Journal of Nutrition.2022; 128(9): 1700. CrossRef - High Density Lipoprotein Reduces Blood Pressure and Protects Spontaneously Hypertensive Rats Against Myocardial Ischemia-Reperfusion Injury in an SR-BI Dependent Manner
Aishah Al-Jarallah, Fawzi Babiker
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Association between the Uric Acid to High Density Lipoprotein Cholesterol Ratio and Systolic Pressure in Chinese Short Stature Children and Adolescents
广欣 李
Advances in Clinical Medicine.2022; 12(09): 8266. CrossRef - Associations Between Peripheral Blood Microbiome and the Risk of Hypertension
Yang Jing, Hui Zhou, Honghong Lu, Xiaofang Chen, Liangyue Zhou, Jingqi Zhang, Jing Wu, Chen Dong
American Journal of Hypertension.2021; 34(10): 1064. CrossRef - How was the Diabetes Metabolism Journal added to MEDLINE?
Hye Jin Yoo
Science Editing.2020; 7(2): 201. CrossRef
- The Association of HDL2b with Metabolic Syndrome Among Normal HDL-C Populations in Southern China
- Epidemiology
- Predictors of Incident Type 2 Diabetes Mellitus in Japanese Americans with Normal Fasting Glucose Level
- You-Cheol Hwang, Wilfred Y. Fujimoto, Steven E. Kahn, Donna L. Leonetti, Edward J. Boyko
- Diabetes Metab J. 2018;42(3):198-206. Published online April 25, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0100
- 3,256 View
- 29 Download
- 5 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Little is known about the natural course of normal fasting glucose (NFG) in Asians and the risk factors for future diabetes.
Methods A total of 370 Japanese Americans (163 men, 207 women) with NFG levels and no history of diabetes, aged 34 to 75 years, were enrolled. Oral glucose tolerance tests were performed at baseline, 2.5, 5, and 10 years after enrollment.
Results During 10 years of follow-up, 16.1% of participants met criteria for diabetes diagnosis, and 39.6% of subjects still had NFG levels at the time of diabetes diagnosis. During 5 years of follow-up, age (odds ratio [OR], 1.05; 95% confidence interval [CI], 1.01 to 1.10;
P =0.026) and family history of diabetes (OR, 3.24; 95% CI, 1.42 to 7.40;P =0.005) were independently associated with future diabetes diagnosis; however, fasting glucose level was not an independent predictor. During 10 years of follow-up, family history of diabetes (OR, 2.76; 95% CI, 1.37 to 5.54;P =0.004), fasting insulin level (OR, 1.01; 95% CI, 1.00 to 1.02;P =0.037), and fasting glucose level (OR, 3.69; 95% CI, 1.13 to 12.01;P =0.030) were associated with diabetes diagnosis independent of conventional risk factors for diabetes.Conclusion A substantial number of subjects with NFG at baseline still remained in the NFG range at the time of diabetes diagnosis. A family history of diabetes and fasting insulin and glucose levels were associated with diabetes diagnosis during 10 years of follow-up; however, fasting glucose level was not associated with diabetes risk within the relatively short-term follow-up period of 5 years in subjects with NFG.
-
Citations
Citations to this article as recorded by- J-shape relationship between normal fasting plasma glucose and risk of type 2 diabetes in the general population: results from two cohort studies
Linfeng He, Wenbin Zheng, Zeyu Li, Lu Chen, Wen Kong, Tianshu Zeng
Journal of Translational Medicine.2023;[Epub] CrossRef - Fasting plasma glucose and risk of type 2 diabetes mellitus in a group of Chinese people with normoglycemia and without obesity
Ziqiong Wang, Zheng Liu, Sen He
Journal of Diabetes.2021; 13(7): 601. CrossRef - Hidden Risks behind Normal Fasting Glucose: Is It Significant?
Seung-Hwan Lee
Diabetes & Metabolism Journal.2018; 42(3): 196. CrossRef
- J-shape relationship between normal fasting plasma glucose and risk of type 2 diabetes in the general population: results from two cohort studies
- Complications
- Hypoglycemia: Culprit or Bystander?
- You-Cheol Hwang
- Diabetes Metab J. 2016;40(3):190-191. Published online June 20, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.190
- 2,510 View
- 26 Download
- Others
- Comparison of the Usefulness of the Updated Homeostasis Model Assessment (HOMA2) with the Original HOMA1 in the Prediction of Type 2 Diabetes Mellitus in Koreans
- Young Seok Song, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
- Diabetes Metab J. 2016;40(4):318-325. Published online May 27, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.4.318
- 4,368 View
- 81 Download
- 39 Web of Science
- 42 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The original homeostasis model assessment (HOMA1) and the updated HOMA model (HOMA2) have been used to evaluate insulin resistance (IR) and β-cell function, but little is known about the usefulness of HOMA2 for the prediction of diabetes in Koreans. The aim of this study was to demonstrate the usefulness of HOMA2 as a predictor of type 2 diabetes mellitus in Koreans without diabetes.
Methods The study population consisted of 104,694 Koreans enrolled at a health checkup program and followed up from 2001 to 2012. Participants were divided into a normal glucose tolerance (NGT) group and a pre-diabetes group according to fasting glucose and glycosylated hemoglobin levels. Anthropometric and laboratory data were measured at the baseline checkup, and HOMA values were calculated at the baseline and follow-up checkups. The hazard ratios (HRs) of the HOMA1 and HOMA2 values and the prevalence of diabetes at follow-up were evaluated using a multivariable Cox proportional hazards model and Kaplan-Meier analysis.
Results After adjusting for several diabetes risk factors, all of the HOMA values except 1/HOMA1-β and 1/HOMA2-β in the NGT group were significant predictors of the progression to diabetes. In the NGT group, there was no significant difference in HOMA1-IR (HR, 1.09; 95% confidence interval [CI], 1.04 to 1.14) and HOMA2-IR (HR, 1.11; 95% CI, 1.04 to 1.19). However, in the pre-diabetes group, 1/HOMA2-β was a more powerful marker (HR, 1.29; 95% CI, 1.26 to 1.31) than HOMA1-IR (HR, 1.23; 95% CI, 1.19 to 1.28) or 1/HOMA1-β (HR, 1.14; 95% CI, 1.12 to 1.16). In the non-diabetic group (NGT+pre-diabetes), 1/HOMA2-β was also a stronger predictor of diabetes (HR, 1.27; 95% CI, 1.25 to 1.29) than HOMA1-IR (HR, 1.14; 95% CI, 1.12 to 1.15) or 1/HOMA1-β (HR, 1.13; 95% CI, 1.11 to 1.14).
Conclusion HOMA2 is more predictive than HOMA1 for the progression to diabetes in pre-diabetes or non-diabetic Koreans.
-
Citations
Citations to this article as recorded by- Non-linear associations of HOMA2-IR with all-cause mortality in general populations: insights from NHANES 1999–2006
Aikai Zhang, Lingchen Huang, Min Tang
BMC Public Health.2024;[Epub] CrossRef - An acute exercise at low to moderate intensity attenuated postprandial lipemia and insulin responses
Lisa L. Ji, Vicki S. Fretwell, Abel Escamilla, Wanxiang Yao, Tianou Zhang, Meizi He, John Q. Zhang
Journal of Exercise Science & Fitness.2024; 22(1): 14. CrossRef - Insufficient compensatory pancreatic β-cells function might be closely associated with hyperuricemia in U.S. adults: evidence from the National Health and Nutrition Examination Survey
Tianran Shen, Qiutong Zheng, Liling Zhong, Xia Zeng, Xiaojing Yuan, Fengxin Mo, Shiheng Zhu, Wenhan Yang, Qingsong Chen
BMC Public Health.2024;[Epub] CrossRef - Glycated haemoglobin, HOMA2‐B, C‐peptide to glucose ratio and type 2 diabetes clusters as predictors for therapy failure in individuals with type 2 diabetes without insulin therapy: A registry analysis
Faisal Aziz, Christoph Sternad, Caren Sourij, Lisa Knoll, Harald Kojzar, Anna Schranz, Alexandra Bürger, Harald Sourij, Felix Aberer
Diabetes, Obesity and Metabolism.2024; 26(3): 1082. CrossRef - Nghiên cứu tương quan giữa chỉ số đề kháng insulin và chỉ số khối cơ thể ở bệnh nhân tiền đái tháo đường có tăng huyết áp
Linh Dương
Journal of Clinical Medicine- Hue Central Hospital.2024;[Epub] CrossRef - Bridelia ferruginea inhibits key carbohydrate digesting enzyme and intestinal glucose absorption and modulates glucose metabolism in diabetic rats
Olajumoke Oyebode, Lindiwe Zuma, Ochuko Lucky Erukainure, Neil Koorbanally, Md. Shahidul Islam
Archives of Physiology and Biochemistry.2023; 129(3): 671. CrossRef - Impact of Pancreatic β-Cell Function on Clopidogrel Responsiveness and Outcomes in Chinese Nondiabetic Patients Undergoing Elective Percutaneous Coronary Intervention
Xiliang Zhao, Jin Wang, Quan Li, Yicong Ye, Yong Zeng
Cardiovascular Drugs and Therapy.2023; 37(3): 487. CrossRef - Development and validation of an insulin resistance model for a population without diabetes mellitus and its clinical implication: a prospective cohort study
Shang-Feng Tsai, Chao-Tung Yang, Wei-Ju Liu, Chia-Lin Lee
eClinicalMedicine.2023; 58: 101934. CrossRef - Association of the triglyceride‐glucose index with subclinical left ventricular dysfunction in type 2 diabetes mellitus patients: A retrospective cross‐sectional study
Qi‐chao Sun, Jie Liu, Ran Meng, Ning Zhang, Jing Yao, Fan Yang, Da‐long Zhu
Journal of Diabetes Investigation.2023; 14(8): 953. CrossRef - Fasting indices of glucose-insulin-metabolism across life span and prediction of glycemic deterioration in children with obesity from new diagnostic cut-offs
Maximiliane Chiara Hammel, Robert Stein, Jürgen Kratzsch, Mandy Vogel, Alexander J. Eckert, Rima Destya Triatin, Marco Colombo, Christof Meigen, Ronny Baber, Juraj Stanik, Ulrike Spielau, Anette Stoltze, Kerstin Wirkner, Anke Tönjes, Harold Snieder, Reinh
The Lancet Regional Health - Europe.2023; 30: 100652. CrossRef - The role of bariatric surgery on beta-cell function and insulin resistance in patients with nonalcoholic fatty liver disease and steatohepatitis
Adisa Poljo, Stephan Kopf, Alba Sulaj, Stephanie Roessler, Thomas Albrecht, Benjamin Goeppert, Sarah Bojko, Beat P. Müller-Stich, Adrian T. Billeter
Surgery for Obesity and Related Diseases.2023; 19(12): 1421. CrossRef - Glutamine Defended the Kidneys Versus Lead Intoxication Via Elevating Endogenous Antioxidants, Reducing Inflammation and Carbonyl Stress, as well as Improving Insulin Resistance and Dyslipidemia
Sina Mahdavifard, Najafzadeh Nowruz
Biological Trace Element Research.2023;[Epub] CrossRef - Sex and genetic background define the metabolic, physiologic, and molecular response to protein restriction
Cara L. Green, Heidi H. Pak, Nicole E. Richardson, Victoria Flores, Deyang Yu, Jay L. Tomasiewicz, Sabrina N. Dumas, Katherine Kredell, Jesse W. Fan, Charlie Kirsh, Krittisak Chaiyakul, Michaela E. Murphy, Reji Babygirija, Gregory A. Barrett-Wilt, Joshua
Cell Metabolism.2022; 34(2): 209. CrossRef - Associations of the HOMA2‐%B and HOMA2‐IR with progression to diabetes and glycaemic deterioration in young and middle‐aged Chinese
Baoqi Fan, Hongjiang Wu, Mai Shi, Aimin Yang, Eric S. H. Lau, Claudia H. T. Tam, Dandan Mao, Cadmon K. P. Lim, Alice P. S. Kong, Ronald C. W. Ma, Elaine Chow, Andrea O. Y. Luk, Juliana C. N. Chan
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - Triglyceride and glucose index is a simple and easy‐to‐calculate marker associated with nonalcoholic fatty liver disease
Kyung‐Soo Kim, Sangmo Hong, Hong‐Yup Ahn, Cheol‐Young Park
Obesity.2022; 30(6): 1279. CrossRef - Protective effect of acetylcysteine, histidine, and their combination against diabetes vascular complications in type-2 diabetic rats via reducing NF-kβ pathway signaling
Sina Mahdavifard, Manochehr Nakhjavani
Journal of Diabetes & Metabolic Disorders.2022; 21(2): 1233. CrossRef - Visceral fat might impact left ventricular remodeling through changes in arterial stiffness in type 2 diabetes: A cross-sectional study
Haishan Huang, Jing Jin, Yanshan Chen, Lina Wang, Jingyi Zhong, Zhenguo Chen, Lingling Xu
International Journal of Cardiology.2022; 368: 78. CrossRef - The effect of berberine and fenugreek seed co-supplementation on inflammatory factor, lipid and glycemic profile in patients with type 2 diabetes mellitus: a double-blind controlled randomized clinical trial
Shima Nematollahi, Gholam Reza Pishdad, Mehrnoosh Zakerkish, Foroogh Namjoyan, Kambiz Ahmadi Angali, Fatemeh Borazjani
Diabetology & Metabolic Syndrome.2022;[Epub] CrossRef - Association between changes in pancreatic morphology and vascular complications in subjects with type 2 diabetes mellitus: a retrospective study
Yuichiro Iwamoto, Tomohiko Kimura, Fuminori Tatsumi, Toshitomo Sugisaki, Masato Kubo, Erina Nakao, Kazunori Dan, Ryo Wamata, Hideyuki Iwamoto, Kaio Takahashi, Junpei Sanada, Yoshiro Fushimi, Yukino Katakura, Masashi Shimoda, Shuhei Nakanishi, Tomoatsu Mun
Scientific Reports.2022;[Epub] CrossRef - Clustering patterns of metabolic syndrome: A cross-sectional study in children and adolescents in Kyiv
Maiia H. Aliusef, Ganna V. Gnyloskurenko, Alina V. Churylina, Inga O. Mityuryayeva
Frontiers in Pediatrics.2022;[Epub] CrossRef - Circulating spexin levels are influenced by the glycemic status and correlated with pancreatic β-cell function in Chinese subjects
Jiarong Dai, Yunzhi Ni, Di Wu, Yaojing Jiang, Shuoshuo Jin, Shan Zhang, Xuemei Yu, Rui Liu
Acta Diabetologica.2022; 60(2): 305. CrossRef - Association between the triglyceride–glucose index and diabetic nephropathy in patients with type 2 diabetes: A cross‐sectional study
Li Liu, Rui Xia, Xiaoqing Song, Benping Zhang, Wentao He, Xinrong Zhou, Shengzhong Li, Gang Yuan
Journal of Diabetes Investigation.2021; 12(4): 557. CrossRef - The insulin resistance by triglyceride glucose index and risk for dementia: population-based study
Sangmo Hong, Kyungdo Han, Cheol-Young Park
Alzheimer's Research & Therapy.2021;[Epub] CrossRef - Determinants of type 2 diabetes remission after bariatric surgery in obese Japanese patients: a retrospective cohort study
Masahiro Ohira, Yasuhiro Watanabe, Takashi Yamaguchi, Atsuhito Saiki, Shoko Nakamura, Shou Tanaka, Naomi Shimizu, Taiki Nabekura, Takashi Oshiro, Ichiro Tatsuno
Diabetology International.2021; 12(4): 379. CrossRef - Sakarya Eğitim ve Araştırma Hastanesine Başvuran Hastaların HOMA-IR Değerlerinin Yaş ve Cinsiyet Faktörü Açısından Değerlendirilmesi
Mehmet ÖZDİN, Hayrullah YAZAR, Durhasan MUNDAN
Mustafa Kemal Üniversitesi Tıp Dergisi.2021; 12(42): 1. CrossRef - Feeding pattern, biochemical, anthropometric and histological effects of prolonged ad libitum access to sucrose, honey and glucose-fructose solutions in Wistar rats
Carmen Alejandrina Virgen-Carrillo, Alma Gabriela Martínez Moreno, Juan José Rodríguez-Gudiño, Jessica Elizabeth Pineda-Lozano
Nutrition Research and Practice.2021; 15(2): 187. CrossRef - The effect of curcumin and zinc co‐supplementation on glycemic parameters in overweight or obese prediabetic subjects: A phase 2 randomized, placebo‐controlled trial with a multi‐arm, parallel‐group design
Majid Karandish, Hassan Mozaffari‐khosravi, Seyed Mohammad Mohammadi, Bahman Cheraghian, Maryam Azhdari
Phytotherapy Research.2021; 35(8): 4377. CrossRef - The Association Between Second-Line Oral Antihyperglycemic Medication on Types of Dementia in Type 2 Diabetes: A Nationwide Real-World Longitudinal Study
Won Jun Kim, Jung Hyun Noh, Kyungdo Han, Cheol-Young Park
Journal of Alzheimer's Disease.2021; 81(3): 1263. CrossRef - Personalized Type 2 Diabetes Management Using a Mobile Application Integrated with Electronic Medical Records: An Ongoing Randomized Controlled Trial
Eun-Young Lee, Jae-Seung Yun, Seon-Ah Cha, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Seung-Hyun Ko
International Journal of Environmental Research and Public Health.2021; 18(10): 5300. CrossRef - Enhancement of Serum Myonectin Levels by Progressive Resistance Training in Rats Fed with High-Fat Diet and Sucrose Solution
Alireza Safarzade, Hadi Safarpour
Zahedan Journal of Research in Medical Sciences.2021;[Epub] CrossRef - Pancreatic β-Cell Dysfunction Is Associated with Nonalcoholic Fatty Liver Disease
Xu Chen, Jinghe Xiao, Juan Pang, Shen Chen, Qing Wang, Wenhua Ling
Nutrients.2021; 13(9): 3139. CrossRef - The correlation between serum resistin and toll-like receptor-4 with insulin resistance in hypertensive subjects with or without type 2 diabetes mellitus
Mustafa Al-Taie, Rayah Baban, Mouayed Hamed
Baghdad Journal of Biochemistry and Applied Biological Sciences.2021; 2(04): 203. CrossRef - Significant fibrosis predicts new-onset diabetes mellitus and arterial hypertension in patients with NASH
Javier Ampuero, Rocío Aller, Rocío Gallego-Durán, Javier Crespo, José Luis Calleja, Carmelo García-Monzón, Judith Gómez-Camarero, Joan Caballería, Oreste Lo Iacono, Luis Ibañez, Javier García-Samaniego, Agustín Albillos, Rubén Francés, Conrado Fernández-R
Journal of Hepatology.2020; 73(1): 17. CrossRef - Are the Different Diabetes Subgroups Correlated With All-Cause, Cancer-Related, and Cardiovascular-Related Mortality?
Peng-Fei Li, Wei-Liang Chen
The Journal of Clinical Endocrinology & Metabolism.2020; 105(12): e4240. CrossRef - Avoiding holiday seasonal weight gain with nutrient-supported intermittent energy restriction: a pilot study
Steven P. Hirsh, Marianne Pons, Steven V. Joyal, Andrew G. Swick
Journal of Nutritional Science.2019;[Epub] CrossRef - Peripartum Management of Gestational Diabetes Using a Digital Health Care Service: A Pilot, Randomized Controlled Study
Ji-Hee Sung, Da Young Lee, Kyoung Pil Min, Cheol-Young Park
Clinical Therapeutics.2019; 41(11): 2426. CrossRef - Development of type 2 diabetes mellitus in people with intermediate hyperglycaemia
Bernd Richter, Bianca Hemmingsen, Maria-Inti Metzendorf, Yemisi Takwoingi
Cochrane Database of Systematic Reviews.2018;[Epub] CrossRef - The cut-off values of surrogate measures for insulin resistance in the Korean population according to the Korean Genome and Epidemiology Study (KOGES)
Bongyoung Kim, Hyun Young Choi, Wonhee Kim, Chiwon Ahn, Juncheol Lee, Jae Guk Kim, Jihoon Kim, Hyungoo Shin, Jae Myung Yu, Shinje Moon, Taulant Muka
PLOS ONE.2018; 13(11): e0206994. CrossRef - Testing for HbA1c, in addition to the oral glucose tolerance test, in screening for abnormal glucose regulation helps to reveal patients with early β-cell function impairment
Yu-Hsuan Li, Wayne Huey-Herng Sheu, Wen-Jane Lee, I-Te Lee, Shih-Yi Lin, Wen-Lieng Lee, Kae-Woei Liang, Jun-Sing Wang
Clinical Chemistry and Laboratory Medicine (CCLM).2018; 56(8): 1345. CrossRef - Metabolic clustering of risk factors: evaluation of Triglyceride-glucose index (TyG index) for evaluation of insulin resistance
Sikandar Hayat Khan, Farah Sobia, Najmusaqib Khan Niazi, Syed Mohsin Manzoor, Nadeem Fazal, Fowad Ahmad
Diabetology & Metabolic Syndrome.2018;[Epub] CrossRef - Pancreatic β-Cell Function and Prognosis of Nondiabetic Patients With Ischemic Stroke
Yuesong Pan, Weiqi Chen, Jing Jing, Huaguang Zheng, Qian Jia, Hao Li, Xingquan Zhao, Liping Liu, Yongjun Wang, Yan He, Yilong Wang
Stroke.2017; 48(11): 2999. CrossRef - Association of serum pancreatic derived factor ( PANDER) with beta-cell dysfunction in type 2 diabetes mellitus
Miral M. Shehata, Mohamed M. Kamal, Mohamed H. El-Hefnawy, Hala O. EL-Mesallamy
Journal of Diabetes and its Complications.2017; 31(4): 748. CrossRef
- Non-linear associations of HOMA2-IR with all-cause mortality in general populations: insights from NHANES 1999–2006
- Response: Increased Risk of Hospitalization for Heart Failure with Newly Prescribed Dipeptidyl Peptidase-4 Inhibitors and Pioglitazone Using the Korean Health Insurance Claims Database (
Diabetes Metab J 2015;39:247-52) - Sunghwan Suh, Gi Hyeon Seo, Chang Hee Jung, Mee-Kyoung Kim, Sang-Man Jin, You-Cheol Hwang, Byung-Wan Lee, Jae Hyeon Kim
- Diabetes Metab J. 2015;39(4):350-351. Published online August 17, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.4.350
- 3,245 View
- 29 Download
- Increased Risk of Hospitalization for Heart Failure with Newly Prescribed Dipeptidyl Peptidase-4 Inhibitors and Pioglitazone Using the Korean Health Insurance Claims Database
- Sunghwan Suh, Gi Hyeon Seo, Chang Hee Jung, Mee-Kyoung Kim, Sang-Man Jin, You-Cheol Hwang, Byung-Wan Lee, Jae Hyeon Kim
- Diabetes Metab J. 2015;39(3):247-252. Published online April 22, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.3.247
- 4,003 View
- 35 Download
- 21 Web of Science
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We assessed the association of dipeptidyl peptidase 4 inhibitors (DPP4i) with hospitalization for heart failure (HF) using the Korean Health Insurance claims database.
Methods We collected data on newly prescribed sitagliptin, vildagliptin, and pioglitazone between January 1, 2009 and December 31, 2012 (mean follow-up of 336.8 days) to 935,519 patients with diabetes (518,614 males and 416,905 females) aged 40 to 79 years (mean age of 59.4 years).
Results During the study, 998 patients were hospitalized for primary HF (115.7 per 100,000 patient-years). The incidence rate of hospitalization for HF was 117.7 per 100,000 per patient-years among patients on pioglitazone, 105.7 for sitagliptin, and 135.8 for vildagliptin. The hospitalization rate for HF was greatest in the first 30 days after starting the medication, which corresponded to a significantly higher incidence at days 0 to 30 compared with days 31 to 360 for all three drugs. The hazard ratios were 1.85 (pioglitazone), 2.00 (sitagliptin), and 1.79 (vildagliptin). The incidence of hospitalization for HF did not differ between the drugs for any time period.
Conclusion This study showed an increase in hospitalization for HF in the initial 30 days of the DPP4i and pioglitazone compared with the subsequent follow-up period. However, the differences between the drugs were not significant.
-
Citations
Citations to this article as recorded by- Cardioprotective effects of dipeptidyl peptidase-4 inhibitors versus sulfonylureas in addition to metformin: A nationwide cohort study of patients with type 2 diabetes
Jui Wang, Hon-Yen Wu, Kuo-Liong Chien
Diabetes & Metabolism.2022; 48(3): 101299. CrossRef - Changing Fields-Diabetes Medications Invading the Cardiovascular Space
Lauren D. Breite, Mackenzie Steck, Brandon Tate Cutshall, Samarth P. Shah, Brandon E. Cave
Current Problems in Cardiology.2021; 46(3): 100736. CrossRef - Cardiovascular Safety and Benefits of Noninsulin Antihyperglycemic Drugs for the Treatment of Type 2 Diabetes Mellitus: Part 2
Srikanth Yandrapalli, Aaqib Malik, Adam Horblitt, Gayatri Pemmasani, Wilbert S. Aronow, William H. Frishman
Cardiology in Review.2020; 28(5): 219. CrossRef - Effects of antidiabetic drugs on left ventricular function/dysfunction: a systematic review and network meta-analysis
Da-Peng Zhang, Li Xu, Le-Feng Wang, Hong-Jiang Wang, Feng Jiang
Cardiovascular Diabetology.2020;[Epub] CrossRef - Dipeptidyl peptidase-4 inhibitor compared with sulfonylurea in combination with metformin: cardiovascular and renal outcomes in a propensity-matched cohort study
Kyoung Jin Kim, Jimi Choi, Juneyoung Lee, Jae Hyun Bae, Jee Hyun An, Hee Young Kim, Hye Jin Yoo, Ji A. Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Cardiovascular Diabetology.2019;[Epub] CrossRef - Comparative Cardiovascular Risks of Dipeptidyl Peptidase-4 Inhibitors: Analyses of Real-world Data in Korea
Kyoung Hwa Ha, Bongseong Kim, Hae Sol Shin, Jinhee Lee, Hansol Choi, Hyeon Chang Kim, Dae Jung Kim
Korean Circulation Journal.2018; 48(5): 395. CrossRef - Worsening Heart Failure During the Use of DPP-4 Inhibitors
Milton Packer
JACC: Heart Failure.2018; 6(6): 445. CrossRef - Resistance exercise improves cardiac function and mitochondrial efficiency in diabetic rat hearts
Tae Hee Ko, Jubert C. Marquez, Hyoung Kyu Kim, Seung Hun Jeong, SungRyul Lee, Jae Boum Youm, In Sung Song, Dae Yun Seo, Hye Jin Kim, Du Nam Won, Kyoung Im Cho, Mun Gi Choi, Byoung Doo Rhee, Kyung Soo Ko, Nari Kim, Jong Chul Won, Jin Han
Pflügers Archiv - European Journal of Physiology.2018; 470(2): 263. CrossRef - Do DPP-4 Inhibitors Cause Heart Failure Events by Promoting Adrenergically Mediated Cardiotoxicity?
Milton Packer
Circulation Research.2018; 122(7): 928. CrossRef - Comparative safety for cardiovascular outcomes of DPP-4 inhibitors versus glimepiride in patients with type 2 diabetes
Hyouk-Jun Chin, Jin Hyun Nam, Eui-Kyung Lee, Ju-Young Shin
Medicine.2017; 96(25): e7213. CrossRef - Effects of dipeptidyl peptidase-4 inhibitor in insulin-resistant rats with myocardial infarction
Nattayaporn Apaijai, Tharnwimol Inthachai, Suree Lekawanvijit, Siriporn C Chattipakorn, Nipon Chattipakorn
Journal of Endocrinology.2016; 229(3): 245. CrossRef - The current role of thiazolidinediones in diabetes management
Christos V. Rizos, Anastazia Kei, Moses S. Elisaf
Archives of Toxicology.2016; 90(8): 1861. CrossRef - Alternative Interventions to Prevent Oxidative Damage following Ischemia/Reperfusion
Simón Quetzalcoatl Rodríguez-Lara, Ernesto German Cardona-Muñoz, Ernesto Javier Ramírez-Lizardo, Sylvia Elena Totsuka-Sutto, Araceli Castillo-Romero, Teresa Arcelia García-Cobián, Leonel García-Benavides
Oxidative Medicine and Cellular Longevity.2016; 2016: 1. CrossRef - Lessons learned from cardiovascular outcome clinical trials with dipeptidyl peptidase 4 (DPP-4) inhibitors
Teresa Vanessa Fiorentino, Giorgio Sesti
Endocrine.2016; 53(2): 373. CrossRef - Letter: Increased Risk of Hospitalization for Heart Failure with Newly Prescribed Dipeptidyl Peptidase-4 Inhibitors and Pioglitazone Using the Korean Health Insurance Claims Database (Diabetes Metab J2015;39:247-52)
Dae Ho Lee
Diabetes & Metabolism Journal.2015; 39(4): 348. CrossRef - Response: Increased Risk of Hospitalization for Heart Failure with Newly Prescribed Dipeptidyl Peptidase-4 Inhibitors and Pioglitazone Using the Korean Health Insurance Claims Database (Diabetes Metab J2015;39:247-52)
Sunghwan Suh, Gi Hyeon Seo, Chang Hee Jung, Mee-Kyoung Kim, Sang-Man Jin, You-Cheol Hwang, Byung-Wan Lee, Jae Hyeon Kim
Diabetes & Metabolism Journal.2015; 39(4): 350. CrossRef - Cardiovascular, renal and gastrointestinal effects of incretin-based therapies: an acute and 12-week randomised, double-blind, placebo-controlled, mechanistic intervention trial in type 2 diabetes
Mark M Smits, Lennart Tonneijck, Marcel H A Muskiet, Trynke Hoekstra, Mark H H Kramer, Indra C Pieters, Djuna L Cahen, Michaela Diamant, Daniël H van Raalte
BMJ Open.2015; 5(11): e009579. CrossRef - Dipeptidyl Peptidase-4 Inhibitor Alarms: Is Heart Failure Caused by a Class Effect?
Yong-ho Lee
Diabetes & Metabolism Journal.2015; 39(3): 204. CrossRef
- Cardioprotective effects of dipeptidyl peptidase-4 inhibitors versus sulfonylureas in addition to metformin: A nationwide cohort study of patients with type 2 diabetes
- Risk Factors for the Progression of Intima-Media Thickness of Carotid Arteries: A 2-Year Follow-Up Study in Patients with Newly Diagnosed Type 2 Diabetes
- Sang Ouk Chin, Jin Kyung Hwang, Sang Youl Rhee, Suk Chon, You-Cheol Hwang, Seungjoon Oh, Kyu Jeung Ahn, Ho Yeon Chung, Jeong-taek Woo, Sung-Woon Kim, Young Seol Kim, Ja-Heon Kang, In-Kyung Jeong
- Diabetes Metab J. 2013;37(5):365-374. Published online October 17, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.5.365
- 4,780 View
- 31 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Intima-media thickness (IMT) of the carotid arteries is known to have a positive correlation with the risk of cardiovascular disease. This study was designed to identify risk factors affecting the progression of carotid IMT in patients with type 2 diabetes mellitus (T2DM).
Methods Patients with newly diagnosed T2DM with carotid IMT measurements were enrolled, and their clinical data and carotid IMT results at baseline and 2 years later were compared.
Results Of the 171 patients, 67.2% of males and 50.8% of females had abnormal baseline IMT of the left common carotid artery. At baseline, systolic blood pressure, body mass index and smoking in male participants, and fasting plasma glucose and glycated hemoglobin levels in females were significantly higher in patients with abnormal IMT than in those with normal IMT. Low density lipoprotein cholesterol (LDL-C) levels in males and high density lipoprotein cholesterol (HDL-C) levels in females at the 2-year follow-up were significantly different between the nonprogression and the progression groups. Reduction of the United Kingdom Prospective Diabetes Study (UKPDS) 10-year coronary heart disease (CHD) risk score after 2 years was generally higher in the nonprogression group than the progression group.
Conclusion LDL-C levels in males and HDL-C levels in females at the 2-year follow-up were significantly different between participants with and without progression of carotid IMT. Furthermore, a reduction in the UKPDS 10-year CHD risk score appeared to delay the advancement of atherosclerosis. Therefore, the importance of establishing the therapeutic goal of lipid profiles should be emphasized to prevent the progression of carotid IMT in newly diagnosed T2DM patients.
-
Citations
Citations to this article as recorded by- Comparison of the Effectiveness of Low Carbohydrate Versus Low Fat Diets, in Type 2 Diabetes: Systematic Review and Meta-Analysis of Randomized Controlled Trials
Tanefa A. Apekey, Maria J. Maynard, Monia Kittana, Setor K. Kunutsor
Nutrients.2022; 14(20): 4391. CrossRef Nomogram Based on Risk Factors for Type 2 Diabetes Mellitus Patients with Coronary Heart Disease
Rong Shi, Birong Wu, Zheyun Niu, Hui Sun, Fan Hu
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 5025. CrossRef- HMGA1 Mediated High-Glucose-Induced Vascular Smooth Muscle Cell Proliferation in Diabetes Mellitus: Association Between PI3K/Akt Signaling and HMGA1 Expression
Qinghai Zhang, Ling Chen, Zhibo Zhao, Ying Wu, Jing Zhong, Gebo Wen, Renxian Cao, Xuyu Zu, Jianghua Liu
DNA and Cell Biology.2018; 37(4): 389. CrossRef - Relationship between frequency of hypoglycemic episodes and changes in carotid atherosclerosis in insulin-treated patients with type 2 diabetes mellitus
Tomoya Mita, Naoto Katakami, Toshihiko Shiraiwa, Hidenori Yoshii, Nobuichi Kuribayashi, Takeshi Osonoi, Hideaki Kaneto, Keisuke Kosugi, Yutaka Umayahara, Masahiko Gosho, Iichiro Shimomura, Hirotaka Watada
Scientific Reports.2017;[Epub] CrossRef - Impact of carotid atherosclerosis detection on physician and patient behavior in the management of type 2 diabetes mellitus: a prospective, observational, multicenter study
In-Kyung Jeong, Sin-Gon Kim, Dong Hyeok Cho, Chong Hwa Kim, Chul Sik Kim, Won-Young Lee, Kyu-Chang Won, Doo-Man Kim
BMC Cardiovascular Disorders.2016;[Epub] CrossRef - The effect of fibroblast growth factors and advanced glycation end-products on the intima-media complex thickness in patients with coronary heart disease and type 2 diabetes
Ekaterina Vladimirovna Ivannikova, Victor Yurievich Kalashnikov, Olga Mikhailovna Smirnova, Alexander Borisovich Kuznetsov, Сергей Anatolievich Terekhin, Alexander Viktorovich Il'in
Diabetes mellitus.2014; 17(2): 47. CrossRef
- Comparison of the Effectiveness of Low Carbohydrate Versus Low Fat Diets, in Type 2 Diabetes: Systematic Review and Meta-Analysis of Randomized Controlled Trials

 KDA
KDA
 First
First Prev
Prev





